1. Introduction
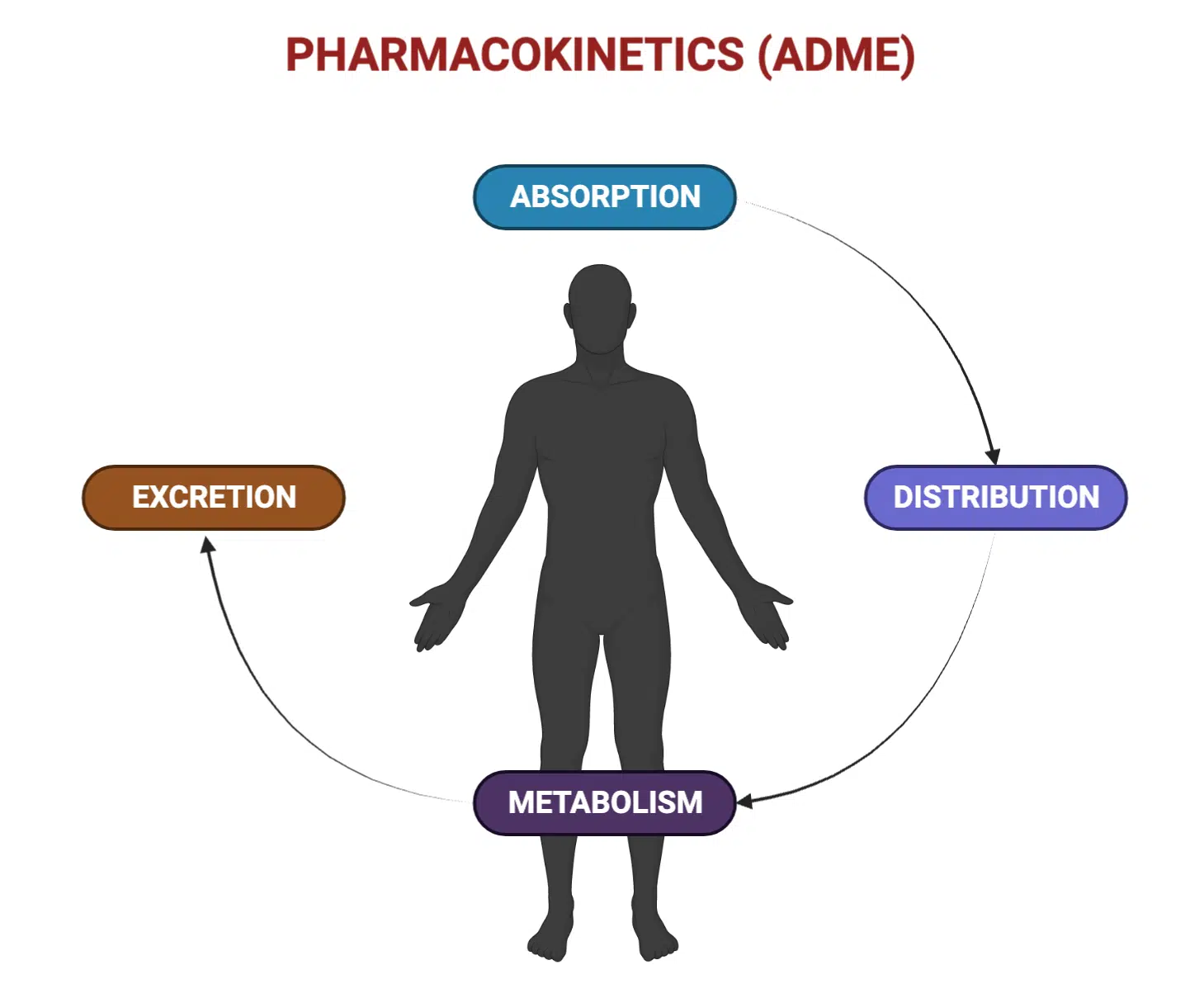
Pharmacokinetics (PK) is the quantitative discipline that describes the temporal journey of drugs through the human body. It addresses four cardinal processes—Absorption, Distribution, Metabolism, and Excretion (ADME)—and provides the mathematical and mechanistic framework needed to answer a quintessential therapeutic question: “What dosing regimen will achieve and maintain drug concentrations that are safe and effective for a specific patient?”
A robust grasp of PK principles underpins rational drug design, regulatory evaluation, clinical dosing strategies, and the burgeoning fields of precision medicine and pharmacogenomics. Whereas pharmacodynamics (PD) elucidates what the drug does to the body, PK clarifies what the body does to the drug. These complementary halves converge in the PK–PD relationship, governing the full therapeutic narrative.
2. Historical Perspective and Evolution
The foundations of PK trace back to the nineteenth-century work of mathematician Johann von Kries and pharmacologist Oswald Schmiedeberg, who first recognized that drug disappearance from blood followed exponential trends. The twentieth century saw classic compartmental models introduced by Torsten Teorell (1937) and expanded by Gibaldi, Wagner, Rowland, and Tozer, who formalized terms such as clearance (CL), volume of distribution (Vd), and half-life (t½).
In the 1990s, advances in computing fostered physiologically based pharmacokinetic (PBPK) modeling, capable of integrating tissue physiology, transporter kinetics, and enzymology to forecast human PK from in-vitro or pre-clinical data. In the twenty-first century, population PK, Bayesian forecasting, microdosing with accelerator mass spectrometry, and real-time biosensor feedback have propelled the field toward individualized therapy.
3. Fundamental ADME Processes
3.1 Absorption
Absorption is the process by which intact drug molecules move from the site of administration into the systemic circulation. Its completeness (extent, reflected by bioavailability F) and rapidity (rate, captured by the absorption-rate constant ka) jointly dictate Cmax and Tmax, shaping both onset and intensity of therapeutic action.
3.1.1 Physicochemical Determinants
- Lipophilicity (log P / log D): greater membrane diffusion but potential for pre-systemic sequestration in adipose tissue.
- Molecular size: small molecules (<500 Da) readily traverse porosity barriers; macromolecules rely on lymphatic uptake or carrier-mediated endocytosis.
- Ionization state: Henderson–Hasselbalch relationships govern pH-dependent partitioning and “ion trapping” across membranes.
3.1.2 Membrane Transport Mechanisms
- Passive diffusion—dominant for lipophilic, non-ionized drugs.
- Facilitated diffusion—transporters such as OATP1B1 mediate hepatic uptake of statins.
- Active transport—energy-dependent efflux (e.g., P-gp) or influx (e.g., PEPT1 for β-lactam antibiotics).
- Endocytosis/pinocytosis—principal for biotherapeutics and nanoparticles.
3.1.3 First-Pass Extraction
Drugs administered orally encounter enzymatic and transporter barriers in enterocytes and hepatocytes prior to reaching systemic circulation. High first-pass extraction drugs (e.g., propranolol, nitroglycerin) may have oral bioavailability below 20 %, necessitating higher oral doses or alternative routes such as sublingual or transdermal delivery.
3.1.4 Non-Oral Routes
- Parenteral (IV, IM, SC): IV offers immediate and complete bioavailability; IM/SC absorption depends on local perfusion and formulation viscosity.
- Mucosal (buccal, intranasal, pulmonary): thin epithelia and high perfusion enable rapid systemic delivery; avoided first-pass metabolism.
- Transdermal: sustained drug release over days; limited to highly potent, lipophilic molecules (e.g., fentanyl, nicotine).
- Rectal: variable; lower rectal veins drain to systemic circulation bypassing the portal vein, providing partial first-pass avoidance.
3.2 Distribution
Distribution describes the reversible transfer of drug from the bloodstream to peripheral tissues until dynamic equilibrium is achieved. Kinetically, it comprises a rapid perfusion-controlled phase followed by slower diffusion-limited equilibration, particularly into adipose and poorly perfused tissues.
3.2.1 Key Influencers
- Tissue perfusion rate: cardiac output fraction dictates the speed at which highly perfused organs (brain, heart, liver) equilibrate.
- Membrane permeability: lipid solubility and tight-junction architecture (e.g., blood–brain barrier) modulate access.
- Plasma-protein binding: albumin for acidic drugs, α1-acid glycoprotein for basic drugs; only the unbound fraction (fu) diffuses and is subject to clearance.
- Tissue binding: sequestration in lysosomes (weak bases), red-blood-cell partitioning (chloroquine), or calcium chelation in bone (tetracyclines).
3.2.2 Apparent Volume of Distribution (Vd)
Vd is a conceptual volume linking the amount of drug in the body to its plasma concentration: V = Dose / C0 (for IV bolus). A small Vd (~0.05 L kg⁻¹) indicates confinement to plasma (e.g., heparin), whereas a very large Vd (>6 L kg⁻¹) suggests extensive tissue binding (e.g., digoxin).
3.3 Metabolism (Biotransformation)
Metabolism converts lipophilic parent compounds into more water-soluble derivatives, facilitating excretion. It occurs predominantly in the liver but also in intestine, lung, kidney, skin, and plasma.
3.3.1 Phase I Reactions
- Oxidation—cytochrome P450 (CYP) family; CYP3A4 handles >30 % of prescribed drugs.
- Reduction—azo-, nitro-, and carbonyl reduction; relevant for prodrugs like chloramphenicol.
- Hydrolysis—esterases and amidases, rapidly cleaving prodrug esters (e.g., remifentanil).
3.3.2 Phase II Reactions
- Glucuronidation—uridine diphosphate-glucuronosyltransferases (UGTs); impaired in neonates (kernicterus risk with chloramphenicol).
- Sulfation—cytosolic sulfotransferases (SULTs); high-affinity, low-capacity route for phenols.
- Acetylation—N-acetyltransferase 2 polymorphism underlies “slow” vs. “fast” isoniazid metabolism.
- Methylation, glutathione conjugation, amino-acid conjugation—important for inactivation of catecholamines and detoxification of electrophilic intermediates.
3.3.3 Enzyme Modulation and Drug Interactions
Potent inducers (rifampicin, carbamazepine) up-regulate CYP expression over days, decreasing substrate exposure. Inhibitors (azoles, macrolides, ritonavir) act rapidly, increasing toxicity risk. Mechanism-based inactivation (grapefruit furanocoumarins on CYP3A4) yields effects lasting beyond inhibitor clearance.
3.3.4 Genetic Polymorphisms
- CYP2D6 gene duplications confer ultrarapid metabolism of codeine → morphine (respiratory depression risk).
- CYP2C19 loss-of-function alleles reduce clopidogrel activation, elevating thrombotic events.
- UGT1A1*28 variant predisposes to irinotecan-induced neutropenia due to impaired SN-38 glucuronidation.
3.4 Excretion
Excretion is the irreversible removal of drug and metabolites from the body, principally via kidneys and bile.
3.4.1 Renal Excretion
- Glomerular filtration: free drug filtered at ~120 mL min⁻¹ in healthy adults.
- Tubular secretion: carrier-mediated; probenecid competitively blocks OAT1/3, prolonging β-lactam half-life.
- Tubular reabsorption: lipid-soluble drugs and unionized species diffuse back; urine alkalinization (sodium bicarbonate) accelerates salicylate clearance.
3.4.2 Biliary and Fecal Elimination
Large molecular weight conjugates (e.g., morphine-6-glucuronide) pass into bile via MRP2, reaching the intestine where bacterial β-glucuronidases can regenerate parent drug, establishing enterohepatic recirculation, manifesting as secondary peaks and prolonged effect.
3.4.3 Minor Routes
Pulmonary exhalation (volatile anesthetics), dermal sweat, saliva, hair (for forensic testing), and breast milk (clinically significant for lithium, amiodarone) constitute ancillary pathways.
4. Quantitative Pharmacokinetics
4.1 Compartmental Modeling
Compartmental models simplify the body into kinetically homogeneous spaces. The one-compartment model assumes instantaneous distribution, leading to mono-exponential concentration decline. The two-compartment model adds a peripheral compartment, yielding a biphasic profile: a distribution (α) phase followed by an elimination (β) phase. Multi-compartment models rarely improve predictive accuracy enough to justify complexity for routine clinical use.
4.2 Physiologically Based PK (PBPK)
PBPK partitions the body into anatomically correct organs, each parameterized by volume, blood flow, membrane permeability, and enzymatic/transporter content. By combining in-vitro intrinsic clearance data with scaling factors, PBPK can: (1) extrapolate animal data to first-in-human doses, (2) simulate special populations (pediatrics, renal impairment), and (3) forecast drug–drug interactions in silico.
4.3 Core Pharmacokinetic Parameters
| Parameter | Definition / Equation | Clinical Implication |
|---|---|---|
| Clearance (CL) | Volume of plasma completely cleared per unit time For IV bolus: CL = Dose / AUC0–∞ | Determines maintenance dose (MD = CL × Css × τ / F) |
| Volume of Distribution (Vd) | V = Dose / C0 (IV bolus) | Guides loading dose (LD = V × Target C / F) |
| Half-life (t½) | t½ = 0.693 × V / CL | Determines dosing interval and time to steady state (≈4–5 × t½) |
| Area Under Curve (AUC) | Integral of concentration-time curve | Metric of systemic exposure; used to establish bioavailability and AUC/MIC indices |
| Cmax / Tmax | Peak concentration / time to peak | Correlate with efficacy (aminoglycosides) or toxicity (theophylline) |
4.4 Multi-Dose and Steady-State Kinetics
With constant-interval dosing, plasma concentration accumulates until input equals output. For drugs obeying first-order elimination, steady state (Css) is reached after 4–5 half-lives, independent of dose magnitude. Fluctuation amplitude depends on dosing interval relative to t½ and on absorption rate. Intravenous infusion achieves Css without peaks and troughs; a loading dose may be employed to attain therapeutic levels rapidly.
4.5 Non-Linear (Michaelis–Menten) Kinetics
When metabolic enzymes approach saturation (C >> Km), elimination becomes capacity-limited. Classic examples—phenytoin, ethanol, salicylate—exhibit disproportionate concentration increments with small dose escalations. The dosing equation transforms to:
Rate of elimination = (Vmax × C) / (Km + C)
For such agents, therapeutic-drug monitoring and cautious dose titration are mandatory.
4.6 Bioavailability and Bioequivalence
Absolute bioavailability (Fabs) compares AUC after extravascular and IV administration. Regulatory bioequivalence between generic and innovator products demands that the 90 % confidence intervals of the geometric mean ratios for AUC and Cmax fall within 0.80–1.25. Modified-release formulations are additionally evaluated for Tmax similarity and “food-effect” robustness.
5. Population Pharmacokinetics and Variability
Population PK employs nonlinear mixed-effects modeling (e.g., NONMEM, Monolix) to partition variability into inter-individual (between subjects), inter-occasion (within subject, between visits), and residual unexplained components. Fixed-effect covariates—body weight, creatinine clearance, genotype, disease status—quantify predictable shifts in CL and V, guiding individualized dosing.
5.1 Demographic Factors
- Neonates and infants: immature CYPs, low UGT activity, high body-water composition; necessitate elongated dosing intervals for renally cleared drugs (e.g., gentamicin q24–48 h).
- Geriatrics: reduced hepatic blood flow and renal function, increased fat-to-lean ratio, frequent polypharmacy; “start low, go slow” dosing ethos.
- Sex: CYP3A4 activity tends to be higher in females; gastric emptying slower, influencing Tmax.
5.2 Organ Dysfunction
- Renal impairment: dose adjust based on creatinine clearance (Cockcroft–Gault) or eGFR; consider dialysis clearance and timing (vancomycin post-HD dosing).
- Hepatic impairment: Child–Pugh score guides avoidance or dose reduction for high-extraction and highly protein-bound drugs; synthetic dysfunction alters albumin and clotting factors affecting PK and PD.
5.3 Pharmacogenomics
- HLA-B*57:01: risk of abacavir hypersensitivity; contraindication if positive.
- VKORC1 and CYP2C9 variants: account for ≈30 % of warfarin dose variability, embedded in dosing algorithms.
- SLCO1B1 c.521T>C: reduced hepatic uptake of simvastatin acid, elevating myopathy risk—dose cap or alternate statin recommended.
5.4 Disease States and Critical Care
Sepsis, burns, cardiogenic shock, and extracorporeal circuits (ECMO, CRRT) dramatically alter Vd, unbound fraction, and organ perfusion, often necessitating real-time TDM and adaptive dosing algorithms.
6. Special Pharmacokinetic Contexts
6.1 Pregnancy
Physiologic changes—↑ plasma volume (40 %), ↑ cardiac output, ↑ GFR (~50 %), ↓ albumin, and altered CYP and UGT activities—generally lower plasma concentrations of renally cleared and CYP3A substrates. Placental transfer favors lipophilic molecules of MW <500 Da; timing of exposure dictates teratogenic risk (organogenesis weeks 3–8).
6.2 Lactation
Drug passage into breast milk is governed by lipophilicity, ionization, protein binding, and milk:plasma ratio. The relative infant dose (RID) <10 % of maternal weight-adjusted dose is deemed low risk; higher RIDs warrant alternatives or feeding schedule adjustment.
6.3 Obesity
In morbid obesity, total body weight (TBW) exaggerates Vd for lipophilic drugs, risking underdosing if ideal body weight (IBW) is used. Adjusted body weight (AdjBW = IBW + 0.4 × [TBW−IBW]) is often applied for aminoglycoside loading; maintenance may follow IBW to prevent accumulation.
6.4 Monoclonal Antibodies and Peptides
- Absorption: subcutaneous bioavailability 60–80 %, mediated by lymphatics; peak plasma in 2–8 days.
- Distribution: confined largely to vascular and interstitial compartments (Vd ≈0.05–0.2 L kg⁻¹).
- Elimination: catabolic proteolysis in reticuloendothelial system; Fc-containing antibodies are salvaged by neonatal Fc receptor, yielding half-lives of 2–3 weeks.
7. Clinical Pharmacokinetic Applications
7.1 Therapeutic Drug Monitoring (TDM)
TDM is pivotal for drugs with narrow therapeutic ranges, variable PK, or concentration-linked efficacy/toxicity. Pre-defined target ranges: digoxin (0.8–2.0 ng mL⁻¹), vancomycin (AUC24/MIC 400–600), lithium (0.6–1.0 mmol L⁻¹). Bayesian software integrates sparse sampling with population priors to individualize dosing.
7.2 Designing Dosing Regimens
- Choose target exposure (e.g., AUC/MIC ≥400 for vancomycin).
- Calculate loading dose if rapid attainment needed: LD = V × Target C / F.
- Compute maintenance dose from clearance: MD = CL × Target C × τ / F.
- Adjust for covariates (renal/hepatic function, weight, genotype).
- Verify with TDM and refine via Bayesian feedback.
7.3 Clinical Vignettes
7.3.1 Gentamicin Once-Daily Therapy
Concentration-dependent bactericidal effect and post-antibiotic suppression permit high-dose (5–7 mg kg⁻¹) extended-interval dosing, targeting peak ≥10 × MIC, trough <0.3 mg L⁻¹. Check level at 6–14 h and apply nomograms (e.g., Hartford) for interval adjustment.
7.3.2 Phenytoin Saturable Elimination
A patient stabilized at 300 mg/day (level 8 µg mL⁻¹) requires upward adjustment. Employ the Michaelis–Menten approximation:
ΔDose = (Vmax × ΔC) / (Cavg + Km)
Typical adult Vmax ≈ 7 mg kg⁻¹ day⁻¹, Km ≈ 4 µg mL⁻¹. Increment of 50 mg may double the level; thus 30 mg increase with re-check in 5–7 days is safer.
7.3.3 Acetaminophen Toxicity
Serum concentration plotted on the Rumack–Matthew nomogram at ≥4 h post-ingestion determines need for N-acetylcysteine. Early ingestion of ethanol (CYP2E1 inducer) accelerates formation of the reactive metabolite NAPQI, lowering the toxic threshold.
7.3.4 Grapefruit Juice Interaction
Single 250 mL serving inhibits intestinal CYP3A4 and P-gp, doubling felodipine AUC for up to 72 h; advise patients to avoid grapefruit when taking high-risk substrates (simvastatin, tacrolimus).
8. Future Directions
Pharmacokinetics is rapidly integrating artificial intelligence, real-time biosensors, nanocarrier design, and systems pharmacology. Point-of-care microsampling (<1 µL blood) and closed-loop infusion pumps are pioneering “adaptive PK,” where dosing is continuously tailored using live data streams. Gene-editing advances may one day modulate drug-metabolizing enzymes directly, redefining PK at its biological roots.
9. Conclusion
Pharmacokinetics provides the quantitative compass that steers every stage of drug therapy—from exploratory molecule to bedside application. Mastery of ADME mechanisms, mathematical descriptors (CL, Vd, t½, AUC), population variability, and special scenarios empowers clinicians and researchers alike to achieve the cardinal therapeutic mandate: deliver the right drug, at the right dose, to the right patient, at the right time.